Iliotibial Band: The IT Band
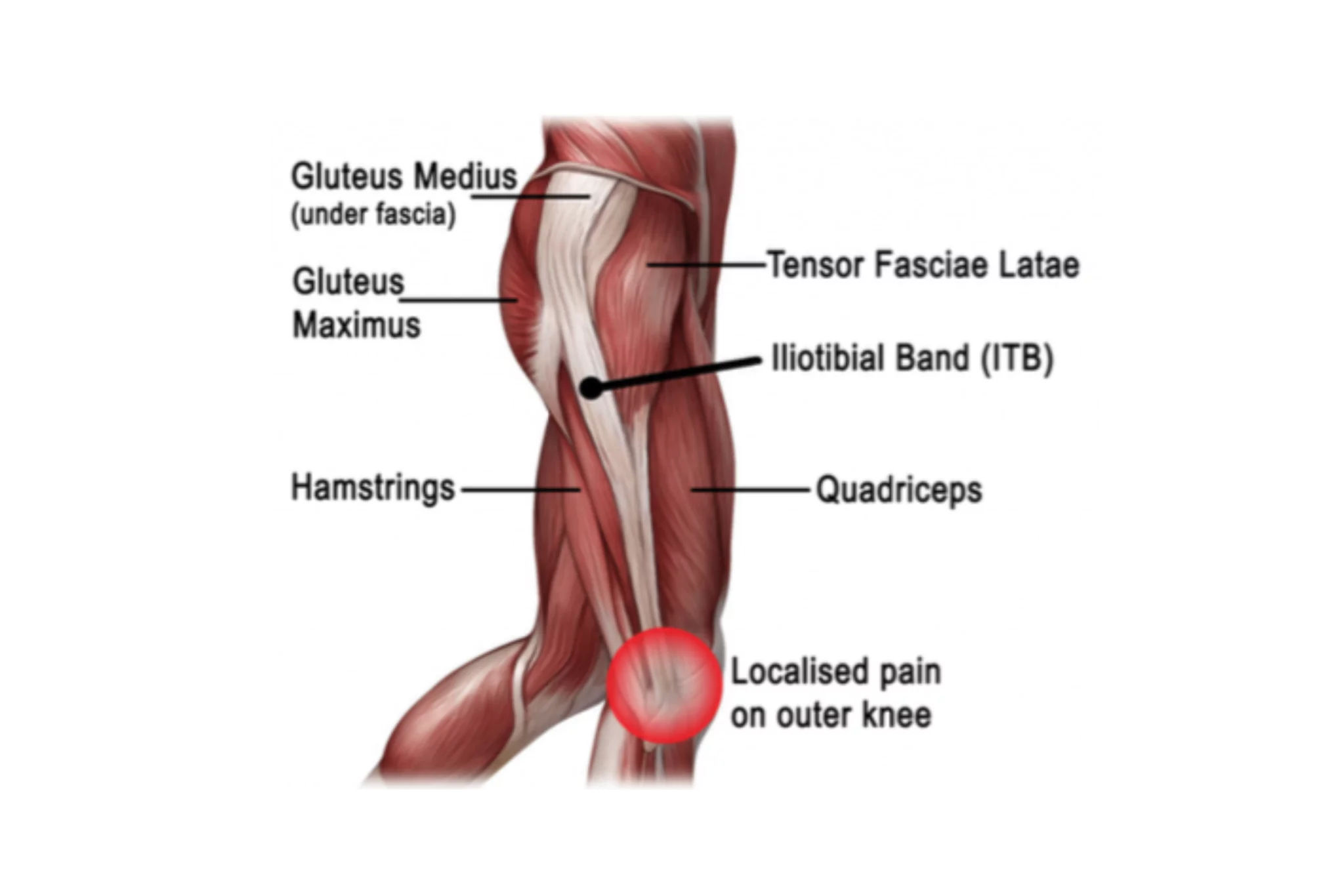
The iliotibial band, also known as the IT band, is a band of fascial tissue. It runs from the iliac crest (top of the lateral aspect of the pelvis) down to the lateral condyle of the tibia at Gerdy’s Tubercle. In other words it runs from the outside of the pelvis, over the hip joint, down the outside of the leg and over the knee joint. It consists of a very thick network of fascial tissue that is extremely fibrous and is good at transmitting force.
At the upper portion of the IT band it interconnects with a muscle called the TFL. TFL contraction and relaxation has a direct effect on the IT band during gait. When the IT band becomes overworked, tight or dysfunctional it can lead to a condition called IT Band Syndrome. ITB Syndrome is among the most common causes of lateral knee pain in runners and can impact cyclists as well.
IT Band syndrome is caused by repetitive knee flexion and extension. Pain happens when the tissue cannot meet the demand of the activity. Contributing factors to IT Band syndrome include but aren’t limited to:
- Increasing running mileage too quickly
- Increased downhill running
- Excessive running in the same direction on the track/road
- Weakness of the hip abductors (lateral Glutes)
- Increased Q angle.
- Tight calf musculature (leads to decreased ankle dorsiflexion, increased pronation and lateral knee valgus)
The common factor in the above causative factors includes too much demand to the tissue. The demand may be too much mileage or improper biomechanics that are causing the IT band to become irritated. It was once thought to be caused by the friction of the IT band rubbing over the femur when you bend your knee. It is now hypothesized that the symptoms come from compression. When you put too much demand on the IT band it tightens up and can apply increased pressure to the tissue between the IT band and the femur. This tissue between the ITB and femur is composed of highly vascularized fat. Highly vascularized simply means that it has a large number of nerve cells and is therefore very sensitive to pressure and pain.
Symptoms of IT band syndrome can vary but typically don’t involve knee joint pain. The pain is typically sharp or burning over the outside of the knee just below the knee joint. During the initial stages of IT band syndrome you may notice symptoms go away shortly after activity. They tend to stick around longer and longer as the injury becomes more severe. A common observation during running or cycling is that the athlete can start their activity pain free. Then at a certain time or mileage they begin to notice the symptoms and it gradually progresses. In addition to the pain there may be snapping, local swelling and crepitus (almost like a crinkly or grinding sound).
Treatment options and concerns:
Treatment for Iliotibial band syndrome is multi-pronged and involves a little bit of trial and error. The first step is to decrease inflammation, typically by icing the area. In addition to icing, conservative care is a large component of recovery. Care includes assessing the tissue health, the biomechanics, and muscular strength of the hip abductors. Once a clear picture is developed, soft tissue therapy is used to help decrease the pressure that is being put on the IT band.
The main tissues of concern with ITB syndrome are the quadriceps, the hamstrings, the calf and popliteus. In addition to soft tissue therapy, strengthening of the lateral hip abductors will help increase the tissue tolerance of the hip abductors. There may also be an additional benefit to strengthening the muscles of the foot. This is because the arch of the foot can collapse with over pronation during running, when this happens it causes the knee to drop in and put extra pressure on the IT band. Strengthening the muscles of the foot or getting orthotics can help prevent the rolling in of the foot. The last component of recovery is activity modification to prevent re-aggravation during recovery.
Changing what is aggravating the injury:
Activity modification is one of the most variable aspects of treatment. Activity modification looks different for everyone based on goals, current mileage, history of running and findings from the assessment. This can look like decreasing mileage, decreasing downhill running, decreasing the speed of runs, decreasing total time running/cycling. Manipulating workouts is all done based when pain starts in activity. This is where seeing a practitioner who has a distinct knowledge of running and cycling can be beneficial to continuing to work towards your goals.
Continuing to train through injuries isn’t always possible. At Connor Chiropractic it is our goal to help you continue to do the things you love. By combining our passion for endurance sports with our experience in run coaching and our in-depth understanding of human anatomy we work to alleviate your pain as quickly as possible.
Looking for somewhere to start to treat or prevent IT band syndrome? These are the some activities that may help start to decrease symptoms
- Stretching out the calf and lower half of the back of the leg
- Strengthening the hip abductors (outside of the pelvis), simple non-weight bearing exercises such as clams or weight bearing exercises such as hip dips
- Strengthening the intrinsic muscles of the foot by lifting up the toes and spreading them or working on lifting the big toe independently from the rest of your toes.
- Hopping up and down on a single leg and not letting your hip drop out under you
It is important to note that these exercises can be beneficial in IT band syndrome recovery but they may not be beneficial in every case. It is helpful when possible to seek an individualized assessment, diagnosis and treatment plan in order to get the most relief as quickly as possible.
Refrences:
- Michael Fredericson et al. Iliotibial Band Syndrome in Runners Innovations in Treatment.USA Sports Med 2005; 35 (5): 451-459 INJURY CLINIC
- John Fairclough et al. The functional anatomy of the iliotibial band during flexion and extension of the knee: implications for understanding iliotibial band syndrome. J. Anat. (2006) 208, pp309–316 © 2006 The Authors Journal compilation © 2006 Anatomical Society of Great Britain and Ireland Blackwell Publishing Ltd